Protons for Patients at Emory - Cancer Treatment with a Big Cost?
/Tej Mehta
Originally published October 14, 2015
photo by: paula tyler
In May of 2013, Emory Healthcare and the Winship Cancer Institute (in partnership with a private funding entity) began construction of the Emory Proton Therapy Center. The $200+ million, 107,000 square-foot facility, which is slated to open in January 2017, will be the first of its kind in Georgia. Based on current construction estimates, the Emory facility will be the 17th operating center nationwide, and will prominently feature new “pencil beam scanning” technology, a major development in the field of proton therapy. The technique itself holds significant promise for many patients in the Emory Healthcare system, but is the potential benefit of proton therapy worth its additional price? The Emory facility has partnered with Advanced Particle Therapy LLC, a proton therapy developer, to help fund the construction and operational expenses.
In 1946, Robert R. Wilson at the Harvard Cyclotron Laboratory, first proposed protons as a therapeutic tool, and the first treatment in the United States occurred in 1954 at the Berkeley Radiation Laboratory. Due to major engineering limitations, proton therapy continued to be used sparingly for many years, predominately for research purposes. In 1989, the first hospital-based center was developed at the Clatterbridge Center for Oncology in the UK, followed by the first US hospital-based center in 1990 at Loma Linda University Medical Center. Since that time, proton therapy centers have been developed at a slow but steady pace, currently numbering 15 operating facilities and an additional 20+ centers under construction. This implies a current access rate of 1 facility for approximately every 20 million US citizens. Globally, there is a dramatic upsurge of interest in proton therapy, with nations like Norway developing widespread access by commencing construction on approximately 1 facility for every 1 million inhabitants.
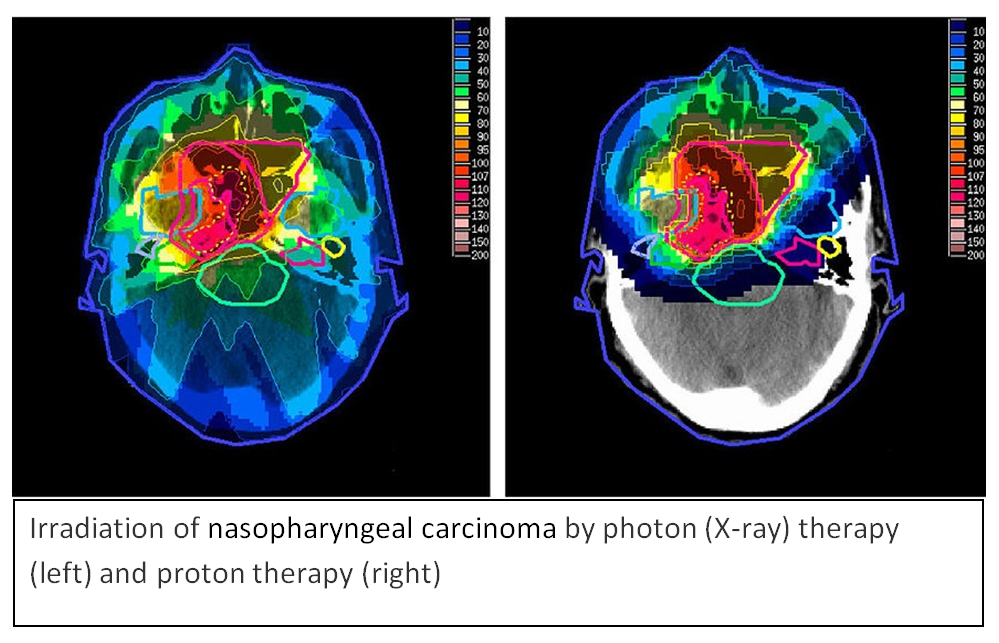
Like other forms of radiotherapy, proton therapy kills cancer cells by causing direct or indirect DNA strand breaks. In modern external beam radiotherapy, tumor-specificity is achieved by physically shaping the beam to minimize exposure of normal tissue to unnecessary radiation; however, because high energy X-rays continue to travel through tissue, some radiation is always deposited in normal tissues in the exit path of these beams. Protons, like high energy X-rays, can also be shaped to match the shape of the tumor, but because of their unique physical property of losing energy while traversing tissue and then depositing all of their energy at a pre-defined depth (based on the initial energy of the beam), there is close to zero exit dose. The result is that while other forms of radiation therapy will deliver radiation to healthy tissue beyond the tumor, proton therapy delivers little to no excess radiation to healthy tissue posterior to the entry beam. This special ability of protons is due to a phenomenon called the “Bragg Peak,” which represents the precipitous and sudden loss in energy that stops protons. Modern proton therapy clinics, such as the Emory facility, also use the previously mentioned technique - pencil-beam scanning - which is analogous to 3-D printing. Like 3-D printing, where thin layers of material are repeatedly applied to make a larger 3-D shape, pencil-beam scanning continuously applies thin layers of protons to a tumor until the entire tumor is treated with radiation. This unique capacity not only eliminates radiation damage past the stopping point of the beam, but also reduces radiation damage to normal tissues all around the tumor. These advantages of proton therapy have been lauded by clinicians and the therapy is generally recognized as particularly useful in patients with a likelihood of long-term survivorship, such as children and young adults. These individuals are typically at greater risk of developing organ dysfunction and secondary cancers as a result of radiation to their normal tissues. Additionally, in situations where an adequate dose to control the tumor simply cannot be safely deposited with conventional modalities, proton therapy is often the best recourse.
Despite these apparent advantages, proton therapy has received significant criticism, both with regards to cost and the level of evidence documenting its true effectiveness. Currently, the primary concern about proton therapy is whether the obvious dosimetric advantages result in “cost-effective” clinical advantages. The upfront construction cost of a multi-room proton therapy facility is well over $100 million, and various analyses have projected that treatment with protons is twice as expensive as X-ray radiotherapy. However, other studies have determined proton therapy to be reasonably priced for most cases, particularly given the potential costs of treating adverse effects caused by standard radiotherapy. For example, one study published in the journal Cancer in 2005 found the average cost of treatment for conventional radiation therapy and proton therapy to be $5,622 and $13,552 respectively. However, the same study found the cost of treating adverse events from conventional radiotherapy and proton therapy to be $44,905 and $5,613 respectively, demonstrating that while the upfront cost of proton therapy may be high, the total costs are significantly reduced.
The other primary criticism against proton therapy is whether or not it is truly as effective as its proponents claim it to be. Thus far, there have been few controlled, randomized clinical trials to demonstrate improved survival or quality of life with proton therapy over other forms of external beam radiotherapy. One such trial randomized patients with ocular melanoma to particle therapy with Helium (similar to proton therapy) against a localized form of radiation known as plaque brachytherapy, and reported superior clinical results for patients on the Helium therapy arm. Several non-randomized trials have supported the clinical benefits of proton therapy. Conversely, detractors of proton therapy point to the lack of randomized clinical trial data as cause for concern with proton therapy, while proponents argue that no clinician has true equipoise to conduct such a randomized trial, stating that to knowingly withhold proton therapy from patients who could benefit from the treatment is unethical. Other critics of proton therapy raise concern over the potential inaccuracy of the exact placement of the Bragg Peak within the tumor. Because of the sudden deposition of energy caused by the Bragg Peak, small errors in measurement or slight movements of the patient could cause a dose-shift. Most modern proton systems deal with this by reducing error through a series of technical refinements, and by performing what is known as “robustness evaluation,” as well as accounting for this uncertainty through a process known as “robustness optimization”.
Emory Healthcare and its affiliates have weighed the costs and benefits of proton therapy and elected to build the facility. The construction of a proton therapy center in Atlanta by Emory Healthcare demonstrates Emory’s conviction to patient care and treatment options and aims to improve the survival and quality of life outcomes of many patients. As the first proton therapy center in Georgia and one of only a handful of treatment centers in the country, Emory has again distinguished itself as a nationwide leader in healthcare.